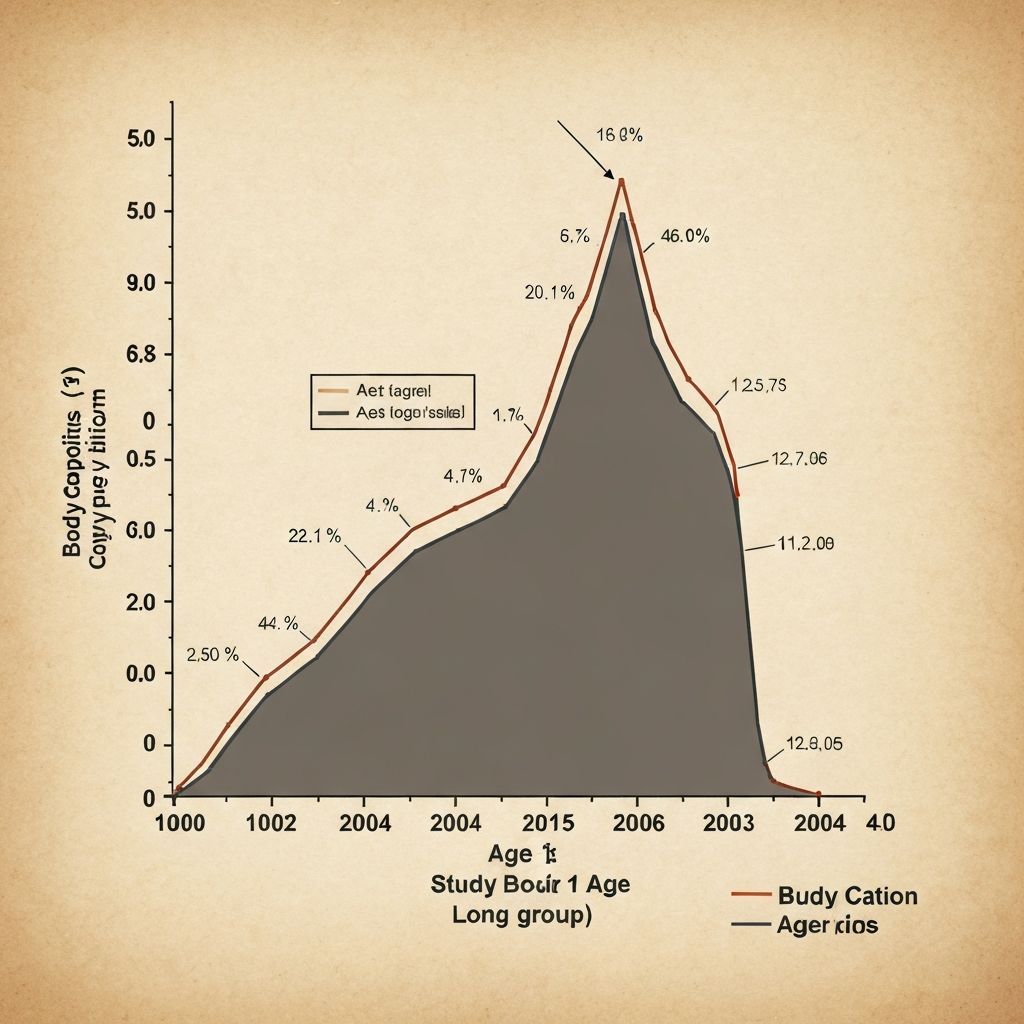
Age-Related Decline in Resting Metabolic Rate
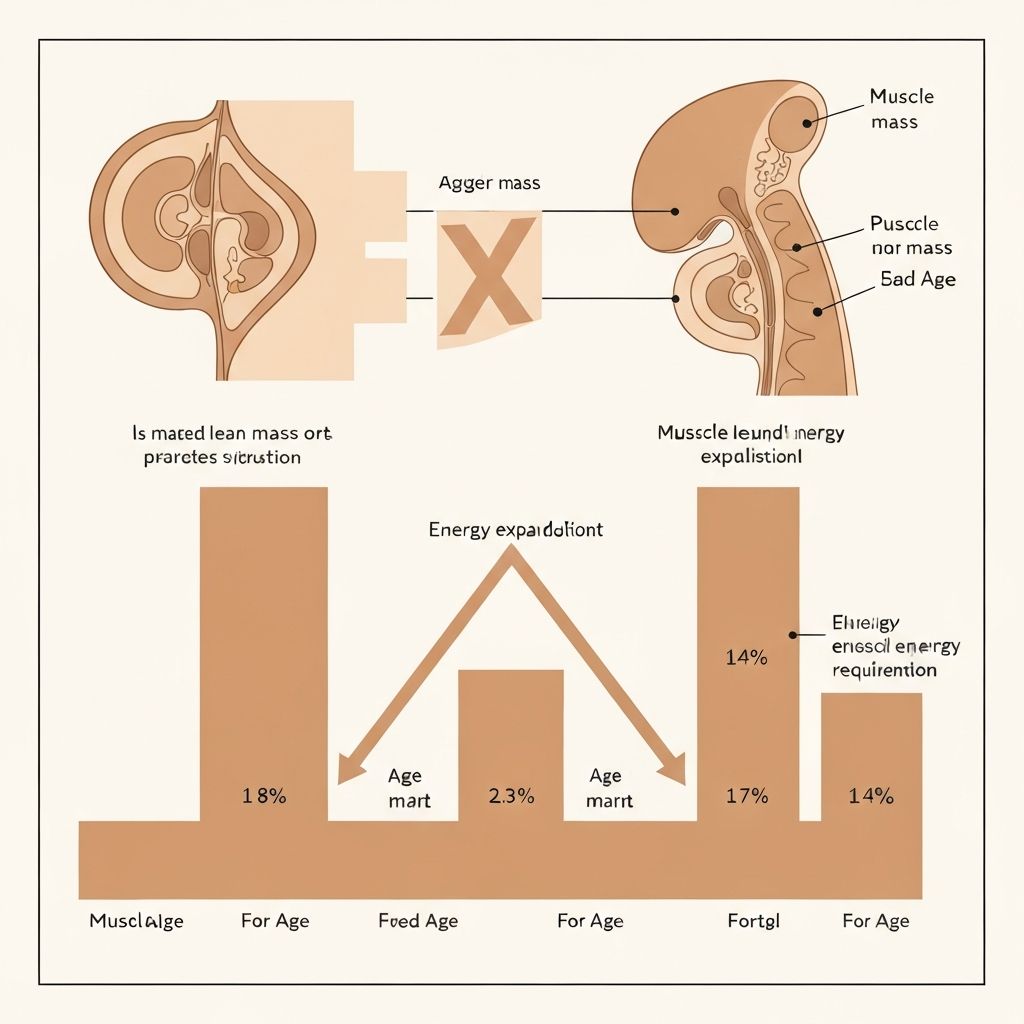
After age 40, resting metabolic rate—the energy your body expends at rest—typically declines gradually. This physiological shift reflects natural changes in body composition and cellular energy production pathways. The decline is not uniform across all individuals and is influenced by multiple factors including activity level, muscle mass distribution, and hormonal changes.
Understanding this mechanism provides context for why energy balance shifts occur during midlife without implying any specific outcome or reversibility. Research consistently documents this pattern across populations, establishing it as a normal physiological observation rather than a condition requiring intervention.